If you experience pain in your clitoris, you are not alone. Clitorodynia, also known as clitoral pain, affects a considerable number of women worldwide. It can range from mild discomfort to severe pain that significantly impacts your quality of life. In this article, we’ll discuss the symptoms, causes, treatment options, natural remedies, prevention measures, and more to help you better understand clitoral pain and manage it effectively.
What is Clitorodynia?
Clitorodynia is an umbrella term for any discomfort, pain, or sensitivity in the clitoris area. It may manifest as a burning, itching, throbbing, stabbing, or shooting sensation, and it can be constant or intermittent. Some women only experience clitoral pain during sexual activity or after orgasm, while others feel it all the time.
Clitorodynia can have a significant impact on a woman’s quality of life, affecting her ability to engage in sexual activity, exercise, or even sit comfortably. It can also lead to anxiety, depression, and other emotional distress. The causes of clitorodynia are not fully understood, but they may include nerve damage, hormonal imbalances, infections, or trauma.
Treatment for clitorodynia depends on the underlying cause and may include medication, physical therapy, or surgery. Women with clitorodynia should seek medical attention to determine the cause of their symptoms and develop an appropriate treatment plan. It is also important for healthcare providers to be aware of clitorodynia and take women’s complaints of clitoral pain seriously, as it is often underdiagnosed and undertreated.
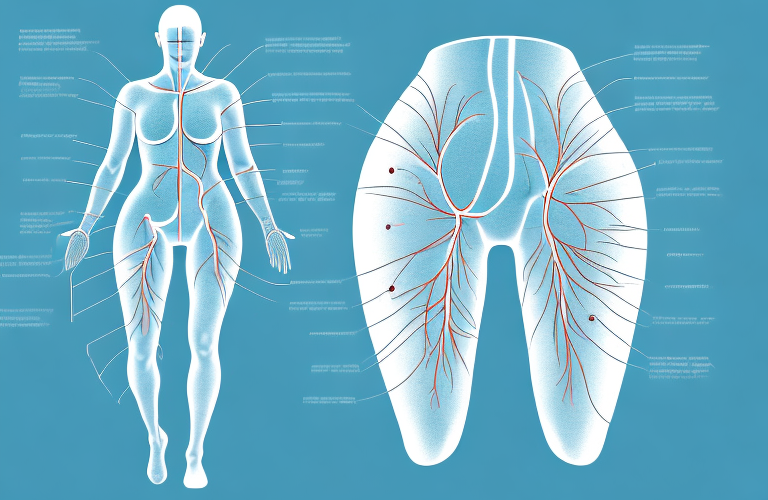
Understanding the Anatomy of the Clitoris
The clitoris is a highly sensitive sexual organ in women that contains thousands of nerve endings. It’s located at the front junction of the labia minora, just above the vaginal opening. The clitoris has two main parts: the external glans and the internal shaft, which extends into the body and meets the crura (legs) near the pubic bone. When aroused, the clitoris fills with blood and becomes more prominent, increasing sensitivity and pleasure.
It’s important to note that the size and shape of the clitoris can vary greatly from person to person. Some women may have a larger or more prominent clitoris, while others may have a smaller or less visible one. Additionally, some women may experience discomfort or pain during clitoral stimulation, which could be a sign of an underlying medical condition. It’s always a good idea to talk to a healthcare provider if you have any concerns about your sexual health or experience pain during sexual activity.
Causes of Clitoral Pain: A Comprehensive Guide
Clitoral pain can be caused by various factors, including but not limited to:
- Physical trauma, injury, or surgery to the clitoris area
- Infections, such as yeast, bacterial vaginosis, or sexually transmitted infections
- Pelvic floor dysfunction, which involves the muscles and ligaments that support the pelvic organs
- Nerve damage or neuropathy, such as vulvodynia or pudendal neuralgia
- Hormonal imbalances or changes, such as during menopause or pregnancy
- Allergies or irritants, such as detergents, tampons, condoms, or lubricants
- Psychological factors, such as anxiety, depression, stress, or trauma
It is important to note that clitoral pain can also be a symptom of underlying medical conditions, such as endometriosis or fibroids. These conditions can cause inflammation and pressure on the clitoris, leading to discomfort or pain.
Additionally, certain medications or treatments, such as chemotherapy or radiation therapy, can also cause clitoral pain as a side effect. It is important to discuss any concerns or symptoms with a healthcare provider to determine the underlying cause and appropriate treatment options.
Types of Clitoral Pain You Should Know About
Clitoral pain can vary in intensity, duration, and quality, depending on the underlying cause. Some common types of clitoral pain include:
- Superficial pain: felt on or near the surface of the clitoris, typically due to irritation, infection, or trauma
- Deep pain: felt inside the clitoris, associated with nerve or muscle conditions
- Referred pain: felt in another area of the body, often due to nerve-related issues
- Provoked pain: triggered by touch, pressure, or movement, commonly seen in pelvic floor disorders or vulvodynia
- Spontaneous pain: occurs without any external stimulation or trigger, seen in nerve or hormonal disorders
It is important to note that clitoral pain can also be caused by psychological factors, such as anxiety or depression. In some cases, the pain may be a result of a past traumatic experience or abuse. It is important to seek professional help if you suspect that your clitoral pain may be related to psychological factors.
If you are experiencing clitoral pain, it is important to talk to your healthcare provider to determine the underlying cause and develop an appropriate treatment plan. Treatment options may include medication, physical therapy, or surgery, depending on the cause and severity of the pain.
Symptoms of Clitorodynia You Cannot Ignore
If you experience any of the following symptoms in your clitoris or vulva, you should seek medical attention as soon as possible:
- Severe, persistent, or worsening pain
- Bleeding, discharge, or foul odor
- Swelling, redness, or warmth
- Rashes, sores, or blisters
- Numbness or tingling
- Difficulty urinating or bowel movements
- Sexual dysfunction or discomfort
It is important to note that clitorodynia can have a significant impact on a person’s quality of life. In addition to physical symptoms, it can also cause emotional distress, anxiety, and depression. Seeking medical attention and receiving proper treatment can help alleviate symptoms and improve overall well-being.
Common Misconceptions About Clitoral Pain
There are several myths and misconceptions surrounding clitoral pain that can make the diagnosis and treatment more challenging. Some common ones include:
- Clitoral pain is always caused by sexually transmitted infections
- Women with clitoral pain cannot or do not enjoy sexual activity
- Clitoral pain is all in the woman’s head or a sign of emotional instability
- Clitoral pain is a rare or imaginary condition that does not require medical attention
However, these misconceptions are not true. Clitoral pain can be caused by a variety of factors, including hormonal imbalances, nerve damage, and physical trauma. It is also possible for women with clitoral pain to still enjoy sexual activity, although they may need to explore different positions or techniques to avoid discomfort.
Furthermore, clitoral pain is a real and common condition that affects many women. It can have a significant impact on their quality of life, including their ability to engage in sexual activity and their overall well-being. Therefore, it is important for women to seek medical attention if they experience clitoral pain, in order to receive an accurate diagnosis and appropriate treatment.
Diagnosis of Clitoral Pain: What to Expect
To diagnose clitoral pain, your healthcare provider may perform a physical exam, ask about your medical history, symptoms, and sexual activity, and order some tests, such as bloodwork, vaginal cultures, or nerve conduction studies. They may also refer you to a specialist, such as a gynecologist, urologist, or pain management physician, depending on the suspected cause.
During the physical exam, your healthcare provider may examine your clitoris and surrounding area for any signs of inflammation, infection, or injury. They may also perform a pelvic exam to check for any abnormalities in the reproductive organs. Additionally, they may ask you to describe your pain, such as its location, intensity, and duration, to help determine the underlying cause.
Depending on the suspected cause of your clitoral pain, your healthcare provider may recommend various treatment options, such as medications, physical therapy, or surgery. They may also suggest lifestyle changes, such as avoiding certain activities or using lubricants during sexual activity. It is important to follow your healthcare provider’s recommendations and attend any follow-up appointments to monitor your progress and adjust your treatment plan as needed.
Treatment Options for Clitoral Pain: Medications, Surgery, and More
The treatment for clitoral pain depends on the underlying cause and severity of symptoms. Some common options include:
- Topical or oral pain relievers, such as lidocaine, gabapentin, or antidepressants
- Antifungal, antibiotic, or antiviral medications, in case of infections
- Muscle relaxants, physical therapy, or biofeedback, for pelvic floor dysfunction
- Surgical interventions, such as nerve decompression or vulvar vestibulectomy, for nerve-related disorders
- Hormonal therapies, such as estrogen or testosterone replacement, for hormonal imbalances
- Cognitive-behavioral therapy, counseling, or support groups, for psychological factors
It is important to note that some cases of clitoral pain may not have a clear underlying cause, making treatment more challenging. In these cases, a combination of different therapies may be necessary to manage symptoms and improve quality of life.
In addition to medical treatments, lifestyle changes can also be helpful in managing clitoral pain. These may include avoiding tight clothing, using lubricants during sexual activity, and practicing relaxation techniques such as yoga or meditation.
Natural Remedies That May Help Relieve Clitoral Pain
While natural remedies may not cure clitoral pain, they can complement conventional treatments and offer some relief. Some examples include:
- Warm or cool compresses, to reduce inflammation and soothe pain
- Herbal supplements, such as turmeric, ginger, or chamomile, with anti-inflammatory or calming properties
- Probiotics or dietary changes, to improve gut and vaginal health
- Avoiding irritants, allergens, or tight-fitting clothes, that can aggravate the symptoms
- Stress-management techniques, such as meditation, yoga, or deep breathing, to alleviate anxiety and tension
It is important to note that natural remedies should not replace medical advice or treatment, especially if the pain is persistent or severe. Consulting a healthcare provider can help identify the underlying cause of clitoral pain and determine the most appropriate course of action.
Additionally, some women may find that incorporating pelvic floor exercises, such as Kegels, into their daily routine can help strengthen the muscles around the clitoris and improve blood flow, which may reduce pain and discomfort.
Coping with Chronic Clitorodynia: Tips and Strategies
If you have chronic clitoral pain, you may need to adopt some lifestyle modifications and coping mechanisms to manage your symptoms effectively. Some practical tips and strategies include:
- Keeping a pain diary, to track your symptoms, triggers, and treatments
- Communicating with your partner or healthcare provider, about your needs and limitations
- Seeking social and emotional support, from family, friends, or online communities
- Scheduling regular self-care, such as massages, baths, or hobbies, to improve your overall well-being
- Engaging in sexual activities that feel pleasurable and comfortable, without forcing yourself to have orgasms or perform certain acts
However, coping with chronic clitorodynia can be a complex and challenging process, and it may require more than just these basic strategies. It is important to consult with a healthcare professional who specializes in sexual pain disorders, to receive a proper diagnosis and personalized treatment plan.
Some additional treatments that may be recommended for chronic clitorodynia include physical therapy, medication, nerve blocks, or surgery. These interventions can help alleviate pain, improve sexual function, and enhance quality of life for individuals with this condition.
Prevention of Clitoral Pain: What You Need to Know
While some causes of clitoral pain are beyond your control, there are some preventive measures you can take to reduce the risk of developing it:
- Practice safe sex, using condoms and avoiding multiple partners
- Maintain good hygiene, by washing your genitals with mild soap and water
- Avoid douching, using scented products, or abrasive clothing
- Kegel exercises, to strengthen your pelvic floor muscles and improve blood flow to the clitoris
- Use water-based lubricants, if needed, during sexual activity, to reduce friction and discomfort
It is important to note that clitoral pain can also be caused by medical conditions such as infections, nerve damage, or hormonal imbalances. If you experience persistent or severe clitoral pain, it is recommended to seek medical attention to determine the underlying cause and receive appropriate treatment.
When to See a Doctor for Clitoral Pain
If you experience any clitoral pain that does not go away on its own or interferes with your daily life, you should seek medical attention. Don’t be shy or embarrassed to discuss your concerns with your healthcare provider, as they are trained to help you and can offer various options for relief. Remember that a healthy and pain-free clitoris is vital for your sexual pleasure and overall well-being.
It is important to note that clitoral pain can be caused by a variety of factors, including infections, injuries, and certain medical conditions. In some cases, the pain may be a symptom of a more serious underlying issue. Therefore, it is crucial to seek medical attention if you experience persistent or severe clitoral pain, as your doctor can help diagnose the underlying cause and provide appropriate treatment.